Latest News
Housing regulations: do the changes affect me?

Housing regulations: What’s changed and how does it affect me?
Dealing with changing housing regulations can be extremely stressful. Our Navigators have provided some information and advice to support you during this difficult time.
During the first lockdown in Spring/Summer 2020, the Government put measures in place to protect tenants from eviction. These were lifted on 20 September 2020, meaning the courts could hear applications for repossession orders.
The same protection has been put in place for the latest national lockdown, meaning renters will continue to be protected from eviction.
The extension to the legislation ensures that bailiffs do not serve eviction notices, except in the most serious circumstances. The only exceptions to this are illegal occupation, false statement, anti-social behaviour, perpetrators of domestic abuse in the social sector, where a property is unoccupied following death of a tenant and serious rent arrears greater than 6 months’ rent.
This legislation will be in place until the end of 21 February 2021 and will be kept under review.
Read the latest guidance for landlords and tenants at GOV.uk
If you Receive Notice
Receiving a notice to quit can be very scary but there are things you can do and help is available. It is important not to ignore the notice but to seek help as soon as you receive it. Your local council has a duty to prevent homelessness so you can approach them for support. They will check the validity of the notice document and can offer to negotiate with your landlord, perhaps to agree a payment plan if there are rent arrears, so you can stay in the property, or help you find somewhere else to live.
If your social housing landlord is serving notice due to rent arrears or ASB you can negotiate a repayment plan with them to reduce the arrears or enter into an ASB agreement. This will allow you to stay in the property as long as you abide by the agreement.
If you are experiencing some of the issues mentioned…
The Navigation team are currently working remotely and are not taking face-to-face appointments but they may be able to support you remotely via telephone and online services.
To refer to our Navigator service, please complete this online referral form or call 020 3317 4200.
This article was originally published in the Autumn/Winter 2020 edition of Community Living Well magazine. To subscribe to receive the magazine, complete this form.
Author: Stewart Gillespie
Category: Community Living Well, Navigator
Posted on: 22nd January 2021
Be kind to yourself during winter lockdown

As we find ourselves in another complete lockdown and are told to ‘stay at home’ to help stop the spread of coronavirus, many of us may find our mental health is deteriorating. It is important to be kind to yourself, so we have rounded up some information, tips and advice on how to cope with certain situations during this time.
Take care of your mental health
You may be getting bored of hearing the same messages like ‘go for a walk’ or ‘learn a new skill’, but activities like this really can help if you’re feeling a certain way.
Get as much sunlight, fresh air and nature
It is scientifically proven that fresh air and natural light can help improve your mood, reduce feelings of stress or anger, and make you feel more relaxed. If you can, go outside for a walk and take in the sights, smells and fresh air.
If you can’t or don’t want to go outside, try opening your windows for a while to let the air in. Listen to natural sounds, like bird song or rainfall – there are apps you can download or videos to watch on YouTube. Spend time in your garden if you have one, or take a break and sit on your front doorstep.
Find ways to fill your time
It’s easy to get bored when you’re stuck indoors so try to find ways to spend your time. You could do some of the things around the house you’ve been meaning to do for ages but never had the time, like having a clear-out or a spring clean.
Relax, read a book or watch TV. It’s ok to relax as well, so don’t be hard on yourself if you decide to do nothing!
Try to keep active
If you can, try to build physical activity into your daily routine. It could be something as simple as walking up and down the stairs or dancing to music. When we feel good physically, we tend to feel more positive and better about life. When we exercise, chemicals such as serotonin and endorphins are released which help to naturally stabilise and lift our mood and improve sleep.
Get a good night’s sleep
If you are struggling to get to sleep because of anxiety or worry about the current situation, try to maintain a regular sleeping pattern and keep up good sleep hygiene practices such as avoiding screens before bed, cutting back on caffeine and creating a restful environment.
Be kind to yourself
It is important to remember that we have made it this far. Since COVID-19 became part of our lives, we have all had to learn and adapt to new ways of living.
Although it might not feel like it, you have achieved more in this past year than you think:
- you’ve adapted
- you’ve shown strength and determination
- you’ve been resilient and patient
They are achievements that you can be proud of.
Other useful information
Seasonal Affective Disorder (SAD) – The advice above can also help if you’re suffering with SAD. Fewer daylight hours plus cold and wet weather means that we can’t spend as much time outside as we did in the first national lockdown. You may feel low in mood and lack motivation.
Read more about SAD, its effects and how to treat it.
Parenting during the pandemic – Having the kids at home can cause more worry for parents if you’re having to juggle working with home-schooling and childcare.
Read our article about parenting during the pandemic, with tips and advice.
Author: Stewart Gillespie
Category: Community Living Well
Posted on: 12th January 2021
Resilience During Uncertain Times
The challenges we’ve faced this year have been extremely tough. The coronavirus pandemic was completely unexpected, and we’ve all had to adapt to a new way of living, whilst trying to remain strong, determined and patient. If you are struggling with your mental health, this uncertainty can bring even more stress and fear.
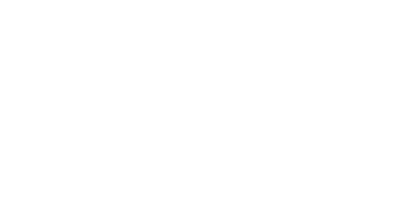
Our Community
Throughout this hard time, it has been wonderful to see friends and family pulling together to support one another and help the community. In Kensington and Chelsea, many voluntary and community organisations, as well as individual volunteers, have been working non-stop to provide people in the community with invaluable support.
We want to highlight the work of some of these incredible people, and say a huge ‘thank you’ to our voluntary heroes…
SMART (St Mary Abbotts Rehabilitation & Training)
SMART begun its food distribution service the day before lockdown started and during their busiest week, they distributed over 270 bags of food. SMART’s neighbours were incredible, popping in to donate food, money or deliver bags. SMART say they were particularly grateful to two young people and their mum who came every week to help out after they had finished their home-schooling.
Director of SMART, Amelia, said, “It has never been just about the food. After every long day of deliveries we would get a flurry of calls, emails and texts from people – ill, frightened, alone – whose world had been brightened by the brief human contact that they had from our volunteers.”
NHS Responders
NHS Responders are a national group of volunteers who provide support to anyone who is shielding, vulnerable, self-isolating or who has caring responsibilities. The volunteers provide various services, including telephone calls to check-in or give support, collection of shopping, medication or other essential supplies, and transport.
Throughout May and June, West London CCG had a total of 2,193 volunteers, who provided 7,698 tasks to 1,345 individuals.
Mutual Aid
Nathan Cooper, Mutual Aid Kensington and Chelsea Volunteer Coordinator, told us about the work they have been doing to help the community:
“In early March, Mutual Aid Kensington and Chelsea was created as a platform to enable neighbourliness in the RBKC. We realised that in this period of unprecedented and uncertain crisis, all residents – regardless of their background – would be affected. Our primary aim was to ensure we could support neighbours to: be kept well fed, have the medicine they need, not have to endanger their vulnerable loved ones by leaving the house, not have to feel alone, and to be able to feel like there’s someone out there listening and looking out for them.
To ensure we were as close to the ground as possible, we formed eight decentralised areas across RBKC, each with its own online communication channels and telephone number so neighbours seeking support could be connected with those offering their time to help out. During the peak of the pandemic, Mutual Aid welcomed around 15,000 volunteers making dozens of food deliveries, running essential errands, and providing health and wellbeing support, working in every RBKC ward, every day. In one ward alone, over 300 calls have led to over 150 support requests being dealt with, all whilst striving for the highest standards of safeguarding and confidentiality.”
To find out how to support Mutual Aid or receive support, please visit MutualAidKC.com or drop us a line on [email protected]
Volunteer Centre Kensington & Chelsea
During the first few months of the pandemic, VCKC received over 2,000 registrations from potential volunteers wanting to help the community. Ahmed was one of those people, and here is his story…
When Ahmed first came to Wellbeing at VCKC (the Volunteering on Prescription team) he was struggling with depression and isolation after having to give up his job due to a health condition. He started to come to community volunteering taster days and to volunteer regularly at his local library and started to feel much happier.
During lockdown, starting in March 2020, he started to feel very isolated and depressed again. Wellbeing phoned Ahmed to assess his needs and started regular Welfare Check phone calls with him. They also liaised with his GP, who was monitoring him carefully. As his mood improved, he has been able to become a wellbeing volunteer and has been helped to access interactive online workshops, such as relaxation, art, and ‘Cook & Chat’. They have also been able to give him some tech support so that he can access his phone therapy sessions.
Recently Ahmed has been helped to facilitate an online wellbeing art workshop. This utilises his artistic skills, which were noted at his initial assessment, and has given him a focus, purpose and sense of pride and satisfaction.
Ahmed said: “I feel more hopeful about the future, I feel very happy. Since I met these people at the Volunteer Centre Kensington and Chelsea, I feel much better.”
Volunteering on Prescription
Volunteering on Prescription is a self-care programme that helps you meet people, share skills and interests and improve your wellbeing through volunteering tailored to your needs. The Volunteer Centre Kensington and Chelsea builds your programme around you and what you like. There is a range of different Self-Care services that can be accessed through Community Living Well.
You can refer to the Self-Care service by completing this online form or call 020 3317 4200.
This article was originally published in the Autumn/Winter 2020 edition of Community Living Well magazine. To subscribe to receive the magazine, complete this form.
Author: Stewart Gillespie
Category: Community Living Well, Self-Care
Posted on: 9th December 2020
Alone in a Digital World

We are living in a fast-paced digital world, where almost everything is now online, including banking, shopping and advice. For many, this is a good thing, as it means faster access to services and instant responses to some requests. But what if you cannot get online? We’ve taken a look at some of the reasons why people can’t get online and provide some tips on how to stay connected if you are feeling excluded.
Digital Exclusion
The recent lockdown has highlighted a major divide in our society, with millions of people unable to access critical online services, and millions more restricted by pay-as-you-go services. This digital exclusion can have an impact on your mental state if you are worried about missing out on vital services such as healthcare, education and benefits.
Did you know…?
13% of UK adults do not use the internet
10% of UK households do not have internet access
65% of smartphone users agree that it is more difficult to complete forms on their smartphone than on a computer
53% of internet users aged 65+ are less likely to bank online
(Source: Ofcom Adults’ Media Use and Attitudes’ report 2020)
Restrictions to access
There are many reasons as to why people do not access the internet:
Accessibility: they might not have access via broadband, WiFi or mobile. Even if they do have an internet connection, they may not have a computer, smartphone or tablet.
Confidence: some are afraid of doing something wrong, lack trust or fear being caught out in an online scam.
Motivation: some people simply do not want to go online.
During lockdown, those with no internet connection or who could not afford to keep topping up pay-as-you-go accounts, were left shut in their homes, socially isolated with no means of contacting anyone in the outside world.
I can’t get online and it’s making me anxious. What can I do?
If you cannot access the internet easily and you’re feeling excluded, support is available.
Make a call
Many services still operate a telephone service – lines may be busier than usual during the pandemic, but you can still get through to speak to someone. Just be patient or try to call at different times during the day.
Seek help or training
Many organisations such as Housing Associations, Local Authorities, Job Centre Plus, and regional health associations can often provide advice, guidance or training.
Ask someone
Find a trusted source – seek help from a friend, family member, carer or health worker. Ask them if you can use their internet access sometimes, or get them to teach you how to use the technology properly.
Other useful information…
This story ‘Alone in a Digital World’ was originally published in the Autumn/Winter 2020 Community Living Well magazine. It has been edited for website purposes. Subscribe today to receive mental health and wellbeing tips straight to your inbox, twice a year!
If you need additional support, you can refer to the Community Living Well service here.
Author: Stewart Gillespie
Category: Community Living Well
Posted on: 2nd December 2020
Autumn/Winter 2020 magazine is now available!
Welcome to the Autumn/Winter 2020 edition of the Community Living Well magazine. We hope you have been keeping safe and well during this difficult time.
The situation regarding Covid-19 and lockdown is changing all the time, which is bringing a lot of uncertainty to our lives. We wanted to include articles that provide practical help and advice on issues that many of us may be dealing with at the moment.
We’ve written an article about suicide prevention to highlight how important it is to talk openly about this – a subject that many of us find challenging. It is vital that we are aware of our own wellbeing, as well as the wellbeing of those around us.
Throughout the pandemic, people have shown courage and resilience – there have been many positive stories to tell, so we focus on some of the incredible voluntary organisations that have helped our community. We also tell you about the ways in which we are continuing to support people using Community Living Well services.
Plus…
The Community Living Well magazine includes information on what to do if you are facing eviction from your home, or if you have been made redundant from your job since lockdown.
If you have any suggestions, features, stories or feedback about the magazine, please contact me, Stewart, at [email protected].
Community Living Well is a mental health service for those registered with a GP in the Royal Borough of Kensington and Chelsea, or the Queen’s Park and Paddington areas of Westminster. The services on offer include talking therapies, support groups, help with employment and support with debt, housing and benefits issues. Self-referrals can be made here. For more information please call 020 3317 4200.
Author: Stewart Gillespie
Category: Community Living Well
Posted on: 6th November 2020
Employment During Second Lockdown
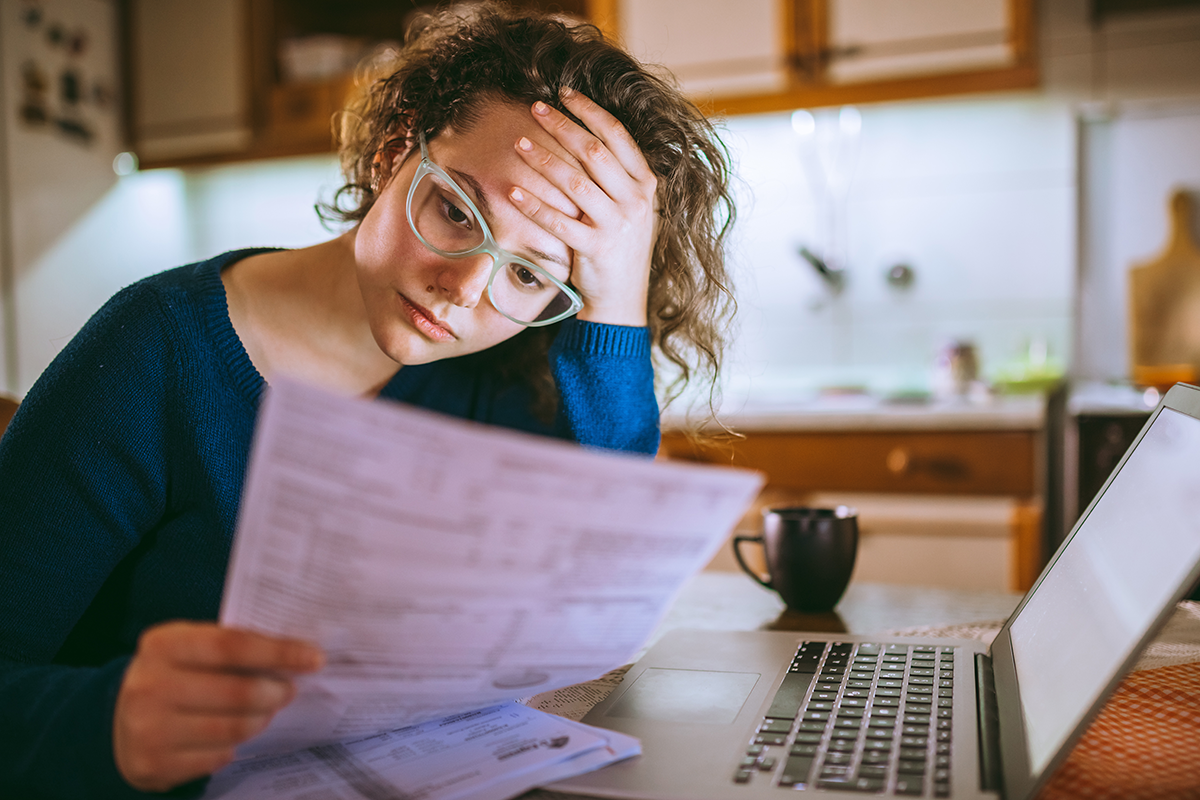
Now that we have entered the second national lockdown of the year, many of us are feeling worried or anxious about the uncertainty of COVID-19 and the affects it is having on our lives. One of the biggest worries comes if you cannot work due to the lockdown restrictions, so we’ve compiled the latest information about furlough, tips on how you can find temporary work and where you can find additional support during lockdown.
GOVERNMENT SUPPORT FOR WORKERS
On Thursday 5 November 2020, the government announced that it would be extending its furlough scheme into Spring 2021, giving businesses and people support during lockdown in the winter months.
The Coronavirus Job Retention Scheme (CJRS) will now run until the end of March with employees receiving 80% of their current salary for hours not worked.
Similarly, if you are self-employed, support through the Self-Employment Income Support Scheme (SEISS) will be increased, with the third grant covering November to January calculated at 80% of average trading profits, up to a maximum of £7,500.
ADDITIONAL SUPPORT
The government also announced that cash grants of up to £3,000 per month are available for businesses which have to close during lockdown, and the mortgage payment holiday for homeowners has also been extended.
For all of the information about the latest announcement, visit gov.uk
LOOKING FOR WORK DURING THE CORONAVIRUS PANDEMIC
Although some businesses have been forced to close until further notice, there are still some who continue to operate by working from home or are considered essential roles.
For non-essential roles, your interview would likely be over the phone or video call. For essential roles such as supermarket assistants, the interview would be face-to-face.
Get in touch with our employment team for some interview tips.
WHERE CAN I FIND WORK?
There may be job opportunities in essential services that must continue to operate during lockdown. Supermarkets might be looking for store assistants, delivery drivers and warehouse workers; you can find opportunities on individual company websites. The NHS have been keen for retired nurses, doctors and healthcare assistants to return, as well as those interested in roles such as porters, cleaners, bed buddies, ward helpers and support workers. These roles are advertised on the NHS Jobs website. Other essential roles include food delivery drivers for companies like Uber Eats and Deliveroo to service those who are self-isolating.
For support with your mental health and wellbeing…
If you are struggling with anxiety, stress or low mood and you feel you need extra support, you can refer yourself to the Community Living Well service here.
Author: Stewart Gillespie
Category: Community Living Well, Employment
Posted on: 6th November 2020
Latest Workshops and Groups

Although we can’t offer our usual face-to-face meetings at the moment, our Talking Therapies and Peer Support teams are offering online alternatives. There is a range of groups, workshops and webinars for you to get involved in if you are feeling anxious, stressed or isolated.
Living Well Workshops
These weekly workshops provide a safe and supportive space to develop skills and knowledge to manage the stresses and difficulties in your life. Each session is different, covering a variety of subjects related to your wellbeing, including Getting a better night’s sleep, Self-care for anxiety, Relaxation and wellbeing, Food and mood, and Stress and wellbeing.
Mental Health Peer Support Groups
These weekly online groups bring people together to give and receive mutual support in a peer support setting, to help manage daily stresses. It’s your chance to talk about your mental health, an opportunity to learn about how others in similar situations manage their symptoms and connect with people who know what it’s like to feel the way you do.
Talking Therapies (IAPT) Webinars
These 4-week courses include Understanding Trauma: supporting clients in having a better understanding of PTSD and to manage symptoms of PTSD that they may be experiencing; Stress Less: supporting clients in understanding generalised anxiety and how it can impact us on a daily basis; and Step Forward: using CBT techniques to increase levels of physical activity in order to reduce symptoms of depression and anxiety.
You can find full details of these and many more upcoming groups on our Events page.
To attend these groups and workshops, you must be registered with Community Living Well. You can refer yourself by completing this online form, or call us on 020 3317 4200.
Author: Stewart Gillespie
Category: Community Living Well, Peer Support, Talking Therapies
Posted on: 29th October 2020
Men’s Mental Health

While many of the same difficulties are experienced by both men and women, there is a difference in the way they address them. Here we look at the importance of men’s mental health and how to support someone who may need it…
Women tend to be more open in discussing their feelings, whereas men have a tendency to keep to themselves and suffer in silence. Quite often they turn to distraction techniques such as spending more time working, drinking more than usual or visiting their ‘man cave’ more often.
A report published by Public First reveals that 28% of men have experienced symptoms of a mental health issue that they believed may require treatment during the last 12 months, but have decided not to seek medical help. Another research conducted by Time to Change revealed that three-quarters of the men surveyed won’t open up to their friends about their mental health struggles and concerns for fear of being a burden. Of those that take their lives in the UK, 75% of them are men.
So why do men choose to suffer in silence?
One of the main reasons is societal gender norms; men should be “tough” and “fearless” and they aren’t really men if they show any sign of weakness. This is called “toxic masculinity”. Some men may also find it difficult to verbalise or even recognise their problems.
Left undetected and untreated, it can lead men to suffer from immense hopelessness, withdrawal and a shutdown of normal activity. It’s important to recognise the signs and encourage each other to speak about how we’re feeling – there’s no shame in feeling vulnerable, lost or sad; everyone experiences these emotions.
How do I support someone who may need it?
- Ask them twice. Some men are unwilling to open up the first time you ask them how they are; but the simple act of asking again shows a genuine willingness to listen and talk.
- Read between the lines. 35% of men have said that if they wanted to talk to a friend about their mental health, they would ask how their friend is doing first and hope they’d ask them back.
- Know when to end the banter. We all like a bit of banter from time to time, but it’s important to know when to stop when someone isn’t in the mood. If you notice a friend is acting differently, ask them how they’re doing. Remember, ‘grow up’ and ‘man up’ are not effective phrases – 42% of men have said these are conversation blockers.
- If he invites you out one-on-one, he may want to chat. 63% of men have said that they would be most comfortable talking about their mental health with someone they trust. Try to just listen and create some space for your friend to share what’s on their mind.
- Let them know they are supported. No need to make it awkward – just let them know you’re there for them. You don’t have to give advice, you just need to be the good friend you’ve always been.
Growing connections through authentic listening and sharing
Peer Support run a men’s group once a month. It’s a safe haven for you to meet other men and hear their stories.
Hearing other men’s stories that resonates with yours can help decrease feelings of loneliness as you get together to talk in an authentic, accepting and non-judgmental way.
To attend the group, you will need to refer to the Peer Support service. Please see below for details on how to refer.
If you would like to find out more about the Men’s Group, please contact 020 3317 4200 or email [email protected].
If you are experiencing any of the issues mentioned…
To refer yourself to the Peer Support service, please complete this online form or call 020 3317 4200.
This story ‘In the spotlight: Men’s Mental Health’ was originally published in the Winter 2020 Community Living Well magazine. It has been edited for website purposes. Subscribe today to receive mental health and wellbeing tips straight to your inbox, four times a year!
Author: Stewart Gillespie
Category: Community Living Well, Peer Support
Posted on: 1st October 2020
Keeping your mind and body fit

We often think of mental and physical health as two separate things, but the truth is, they are very closely linked. When we feel good physically, we tend to feel more positive and better about life – it is important to keep your mind and body fit.
Things that can be good for our physical health can also have a hugely positive impact on our mental health. Keeping active is a very powerful tool for doing this. We are all aware that exercise can improve physical health by making us stronger and reduce the risk of certain diseases. What is less known is that exercise can improve our mental wellbeing; how we feel and our ability to cope with the stresses of day-today life.
What is it about exercise that makes us feel good?
When we exercise, chemicals such as serotonin and endorphins are released which help to naturally stabilise and lift our mood and improve our sleep.
Regular exercise can increase our energy levels throughout the day and even enhance our ability to learn and memorise new things. On top of this, doing physical activity can give us a huge sense of achievement and help us to discover new interests and meet new people.
Often many of us hear the word exercise and panic, thinking we should be running marathons or lifting unearthly weights at the gym, but this isn’t the case!
Exercise can be anything that gets us moving; from doing our weekly shop or cleaning the house to dancing or going for a walk. No matter our age or fitness level, we can all seek the benefits of exercise.
By improving your physical health, it should help with improving your mood and wellbeing!
Need extra support?
We’re here to help. We are still accepting referrals during the current pandemic. We offer the following services:
- Talking Therapies (IAPT) – Short-term support for when you experience difficult emotions, such as, low mood, worry and stress
- Peer Support – Wellbeing workshops, one-to-one peer support, peer support groups, social activities and peer support training with other people who have had similar experiences to you
- Employment – Advice and support to gain and retain paid employment, improve your employability skills and know your rights in the workplace
- Navigators – Practical support with a range of issues including benefits, debt, housing options, access to health and social care services and support to access specialist advice and information
- Self-Care – Support and activities that help you to take care of your own mental, emotional and physical wellbeing
This story ‘Keep your mind and body fit’ was originally published in the Winter 2020 Community Living Well magazine. It has been edited for website purposes. Subscribe today to receive mental health and wellbeing tips straight to your inbox, four times a year!
Refer to the Community Living Well service here.
Author: Stewart Gillespie
Category: Community Living Well, Self-Care
Posted on: 24th September 2020
Sleep and anxiety

There are plenty of benefits to a good night’s sleep. However, we sometimes find ourselves tossing and turning with feelings of dread and unease. If you find yourself in this position, there are some simple things you can do to help manage your sleep and anxiety.
Why can’t I sleep?
Many people suffer from sleep problems, including the inability to fall asleep, regularly waking up during the night and not being able to fall back asleep again, and early waking. The cause of some sleep problems may be related to physical health, for instance the effect of a health condition or medication you are taking. However, often the underlying cause is psychological, for instance symptoms of anxiety, depression or trauma. It is important to seek help from your GP for these underlying psychological problems.
You may be someone who finds that as soon as you lie in bed emotions or thoughts come to the surface. This may be a sign that you’re not attending to these emotions in your waking hours. Make time to know what you’re feeling and try and find an outlet, such as a journal, creating a worry list or talking to others for support.
If this doesn’t improve things, then think about talking to your GP about potentially accessing a talking therapy or you can self-refer to our service.
What can I do to improve my sleep?
Sleep hygiene is a set of good habits that can help improve sleep. Here are some tips and recommendations to help overcome issues with sleep and anxiety:
- Try to go to bed and get up at the same time every day and avoid naps. A regular routine helps train your body for sleep.
- Avoid caffeine and nicotine for four to six hours before bedtime as they are both stimulants that affect your sleep. Instead have some warm milk or chamomile tea.
- Don’t use alcohol to help you sleep. While it may make you sleepy in the immediate short-term, it has a negative effect on the quality of your sleep and can lead to you developing a dependency.
- If you have trouble falling asleep, try to distract yourself with breathing exercises, meditation or deep muscle relaxation.
- Avoid using smartphones, tablets or other electronic devices for an hour or so before you go to bed as the light from the screen may have a negative effect on sleep.
- Try not to clock-watch. A lot of people worry about not getting enough sleep, but watching the clock makes you more tense and anxious, which leads to you being more stimulated and less likely to fall asleep.
- Your bed is for sleeping so try to help entrench this connection by not using it as a place to do other activities, such as watching television, eating or surfing the internet.
- Develop rituals before bedtime. For instance, having a warm bath can help you feel sleep, or do some meditation or stretching exercises.
- A good diet can help with good sleep. Try to avoid heavy meals before bed. However, an empty stomach can be quite distracting so if you’re hungry, have a light snack.
- Your bedroom ideally needs to be dark, quiet, tidy and be kept at a temperature of 18C and 24C
Helpful resources
Sleepio is an online sleep improvement programme based on CBT principles. It’s free for people living in London. Download it here: www.good-thinking.uk/sleepio
Overcoming Insomnia and Sleep Problems: A Self-Help Guide Using Cognitive Behavioral Techniques by Colin A. Espie
If you are experiencing some of the issues mentioned…
If you feel you need additional support to overcome your concerns with sleep and anxiety, our Talking Therapies service may be able to help. You can register for the service by completing this self-referral form.
This story was originally published in the Winter 2020 Community Living Well magazine. It has been edited for website purposes. Subscribe today to receive mental health and wellbeing tips straight to your inbox, four times a year!
Refer to the Community Living Well service here.
Author: Stewart Gillespie
Category: Community Living Well, Talking Therapies, Uncategorised
Posted on: 9th September 2020